By David Buckles, ATC
Alright ladies and gentlemen…I’ve seen more plantar fascia-related injuries come in to the running store than probably almost all other running related injuries PUT TOGETHER!! Why is it so common, what is it, how do I get rid of it, where am I? I’m going to answer all these questions for you shortly. Let’s dive in to the definition of the injury, and then we’ll break in to some sub categories of the injury. Any readers out there, if you’ve found something that has worked for you, please post it in the comments!
More often than not, when you see the suffix “itis” on the end of a word, it usually indicates an inflammation of the root word (ie: tendonitis-inflammation of a tendon, fasciitis- inflammation of a fascia). That’s not always the case though, remember when you were a senior in high school, and you didn’t want to go to classes anymore, everyone said that you had a case of ‘senior-itis’, if this were correct, you would be an inflamed senior… doesn’t always work does it? In the case of the plantar fascia however, it is true.
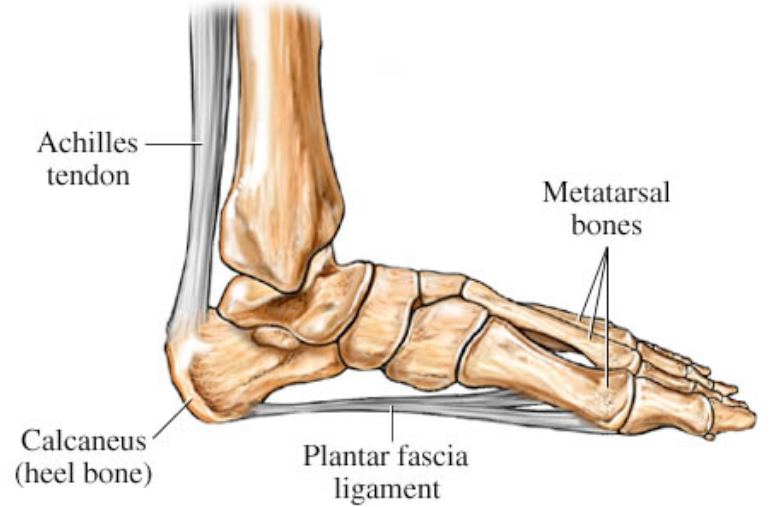
One of the reasons it is so prevalent is because we walk almost everywhere we go. The plantar fascia originates in the foot on the heel on a bony protuberance called the calcaneal tuberosity. It inserts on the heads of each metatarsal. Fascia, by nature, is not very stretchy, but it as STRONG!
The above picture is a diagram of the left foot. The main arch in our feet is known as the medial-longitudinal arch. The arrow indicates the calcaneal tuberosity. Remember that every time we take a step, this arch flexes to a certain extent so that we can absorb impact more efficiently. When that arch in the foot flattens out, the plantar fascia stretches also. Because it is not a very elastic material, it can end up getting irritated, and even ripping in some places. Now try to count the number of steps that you take in a day, each and every day… it becomes easy to see how so many people are plagued by this injury.
Etiology of plantar fasciitis (PFitis)- PFitis can be exacerbated by hyper pronation. If the medial longitudinal arch flattens out too much, and over pronation is evident, this motion puts extreme stretches on the fascia. Tight calves can be a very good indication and a gateway to PFitis rearing its ugly head. Ideally, the plantar fascia is a continuation of the Achilles tendon, if the Achilles is shortened due to tight calf muscles, chances are that your plantar fascia is going to be tight as well. Below is a list of several things that I have seen in the past that have caused or that can cause PFitis:
- Toe Running
- Wearing flip-flops (or other non-supportive sandals)
- Excessive uphill training
- Hyper pronation
- Cussing and smoking (not really, but don’t do these either)
- Lack of supportive inserts within your walking/running shoes
- A dramatic increase in training
Pathology of PFitis– As previously stated, the fascia is not very elastic, when it stretches, it doesn’t give very well, so it can rip in places or become very aggravated. This almost always results in inflammation. A very close friend of PFitis (which usually accompanies it) is an injury known as heel spurs. Due to the fascia’s nature of not being flexible, when it stretches (because it is strong), the fascia itself may not tear, but if may tear bits and pieces off the bone of your calcaneus (heel). This is known as an avulsion fracture. Take a look at the picture below, an x-ray only show the bone, not connective tissue. In this instance, the plantar fascia, due to repeated stretching has pulled pieces of bone off of the calcaneus and the pieces of the heel have re-solidified and created a ‘spur’ off of the heel… painful, right? Now imagine this spur digging in to your plantar fascia every time you take a step… no wonder it’s not healing!!
Evaluation of Plantar fasciitis can usually be relatively easy, albeit painful. A common tell-tale sign is the first few steps out of bed. If the first few steps out of bed in the morning are painful and debilitating, it is a good indicator of PFitis. Here’s a list of things that you should watch out for as far as signs and symptoms are concerned. PFitis is not limited to, nor will it exhibit all of these S&S:
- Point tenderness directly over calcaneal tuberosity
- Pain with initial steps after sleeping all night, or sitting for extended periods of time
- Possible swelling
- Often times loosens up while exercising, but reappears afterwards
- Possible decrease in active range of motion with plantar flexion and dorsi flexion
- Possible weakness with plantar flexion
Prevention of plantar fasciitis can be as easy as ‘1, 2, 3’
- Avoid flip flops and any other sandal with no support. Take a look at your very own arch, is it flat? NO, but flip flops are! I would highly recommend an insert, a sandal, a shoe with something inside of it that contours to your arch. Shoes are flat inside, and the insert that comes with it is too soft and flexible to do you any good. You want something with a higher, more rigid arch that prevents yours from flattening out too much. Just because the outstanding employees at SLRC fit you in a ‘stability’ shoe, doesn’t mean that your medial longitudinal arch height is taken care of, that is where the benefit of inserts come from! Check them out!!
- Stretch out your calves. More often than not, the tighter you are, the more open you leave yourself to tearing something. I know what you’re saying, “Dave, what about the quote that says a lion never stretches before it tackles a gazelle”. Well, for one thing you’re not a lion. Secondly, lions don’t run for miles on end chasing down said gazelle. And lions don’t even have plantar fascia. And ladies… watch out for wearing high heels too often. While wearing high heels, the Achilles tendon shortens up over time, predisposing you to tighter and tighter calves than your male counterparts, watch out!!
- Check your mileage. If you are putting more stress on your fascia than what it is used to, it may rebel against you.
Rehabilitation of such an aggressive injury must be aggressive in and of itself. Depending of the severity of heel spurs that may be accompanying your PFitis, surgery may be required. If your injury is severe (meaning that it causes extreme pain) an x-ray may be crucial! If you remember back to the illiotibial band discussion, you may remember me talking about scar tissue. When a soft tissue such as a muscle, or tendon, or even fascia becomes aggravated and damaged, it usually creates scar tissue to heal itself. This scar tissue does not lay down as congruent as the original fibers did, and the scar tissue is certainly not as malleable. This increase in scar tissue can turn out to be the bane of your existence, so it is imperative that you get rid of it, or massage it out of there.
- The foot wheel (sold at SLRC) can help tremendously. When you are sitting around at the desk, watching television, or what have you, simply roll your foot over this beaded roller and put as much pressure on plantar aspect of your foot as you can stand. The idea behind this is to break up any scar tissue that may be inhibiting flexibility in the fascia. Another great modality to use is a frozen bottle of water. Roll your foot over the bottle the same way, but you get massage and ice at the same time, brilliant!
- The Strassburg sock can help also. Though it is not a permanent solution to curing PFitis, it can make rehabilitation much easier. While sleeping, your fascia is in a relaxed position. When your body is at rest and in a relaxed plantar flexed position (shortened Achilles tendon), it will try to heal itself by sending blood to the affected area and creating scar tissue. Blood platelets temporarily fill in the cracks and tears and rips in your fascia creating a temporary ‘plug’. The fascia is not a very vascular area so it cannot fully heal itself over night. When you take a step the next morning, because the plug is not fully set and healed, BAM, it gets ripped all over again. What the night splint will do, is ensure that you sleep in a dorsi-flexed position. When sleeping in this position, your Achilles is elongated, your fascia is elongated. When that temporary plug is put in overnight, it adheres to a stretched-out soft tissue. When you take that step in the morning, you are no longer ripping every fiber in that tendon and fascia, voila!
- This is my favorite for strengthening the fascia. I would usually wait until you are asymptomatic before you introduce this rehabilitation exercise to your routine, but it helps like nothing else… Read these directions carefully… stand close to a wall. Get up on your tippy toes, and bend your knees. Your goal is to lean forward enough that you have to occasionally push off the wall. The goal is to get as close to the wall without actually ever touching it. Just hover your hands against the wall just in case you need it. If you have done this correctly, you will feel a burn in your arches
- Here are a few other simple rules that may expedite the healing process. Always ice after a workout! Before a workout, throw a heat pad on your fascia. This will encourage more blood flow to the area, and make the fascia and tendon more malleable before exercise. Be careful not to burn or freeze your skin while doing either one of these.
I know I can’t sum up the pain that some of you have experienced in only a few paragraphs, but if you have any questions, or you’re just not sure of anything I said here, or if you want to discuss PFitis in length, feel free to call me at the Draper location 801-676-0844. Thanks for reading, we’ll see you next time, same bat time, same bat channel. (That’s an old batman reference in case you didn’t catch it)