David J Buckles, ATC
Welcome back ladies and gentlemen to another exciting edition of “Oh crap, what have I done to myself.” Today we’re going to look at an issue that seems to target an uncanny amount of runners out there. The injury is called Illiotibial Band Friction Syndrome, or IT Band Syndrome or ITB for short. I usually prefer understanding what an actual structure is, how it works, and how it becomes injured before I learn how to heal it, so that’s what I’m going to make you all do!
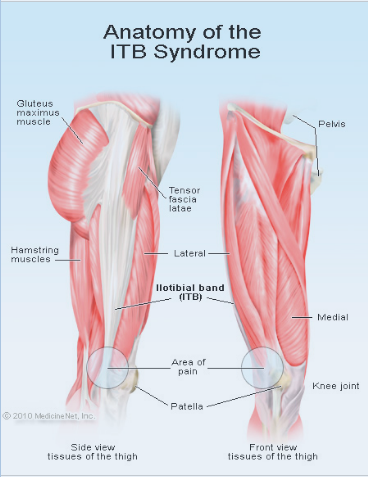
The IT Band is a thick fibrous tissue that originates from a collection of muscles on the outside of your hip and inserts to a bony protuberance just below and outside of your knee called the Gerdy’s Tubercle. There are three muscles associated with the origination point of the IT band, they are the Gluteus Maximus, Gluteus Medius, and Tensor Fascia Latae muscles. If you follow the IT Band down to the tubercle, you will find that it positions itself in front of, or sometimes behind a little knob on your femur bone called a femoral epicondyle. When you bend your knee past 30 degrees the IT Band moves behind the femoral epicondyle. If you were to fully extend your knee, the IT Band moves in front of your femoral epicondyle.
Muscles Tied to the IT Band
Here is a brief overview of what the three muscles at the origination point of the IT Band are responsible for:
Gluteus Maximus(GMAX): Extension of the hip.
Gluteus Medius(GME): Abduction of the hip (a hip stabilizer)
Tensor Fascia Latae (TFL): Abduction of the hip (a hip stabilizer)
Maximus Desimus Meridius: Russell Crowe’s character in Gladiator.
Etiologies of the IT Band
Stable hips are very important to a runner. The GME and TFL are designed to prevent excessive motion of the hips while we are walking and running. If there are deficiencies and weaknesses in these muscles, the hips flop all over the place and we can expect a hip blow-out several years down the road. When we run and our muscles work hard by preventing excessive hip movements, they become tighter and tighter. Because of this, they end up pulling on the IT Band making it taut. When the IT Band becomes tighter, it produces more friction over the femoral epicondyle every time our knee flexes and extends.
- Over pronation can be a contributor of IT Band Syndrome as well. Here’s how: When the foot comes in contact with the ground, the arch flattens out, and tends to pronate to a certain extent. Remember, this is how the body absorbs some shock. If a foot is over-pronated, not only will that runner be on the inside of his/her foot, but the knee moves medially as well. If the knee moves medially, it creates a greater pull on the IT Band. Now imagine you have tight hip muscles, your foot is pronated so your knee moves medially with each step… how much stress is now placed on that Illiotibial band? The answer: LOTS!
- Running downhill can exacerbate this injury. When running downhill, most runner’s strides become longer causing our hips to work so much harder in order to stabilize.
- Women are usually at a greater risk of ITB because of what is referred to as the Q angle. The Q angle represents the angle between the hip, knee cap, and tibial tuberosity.
Pathology of IT Band Syndrome
The IT Band comes in contact with the femoral epicondyle many times during your run. If the IT Band is tight, this contact turns in to something much more painful. When the Band creates friction with the epicondyle, inflammation usually occurs. If the IT Band is inflamed, the chance that it will create more friction when it is engorged becomes very great. Take for example: When you bite your lip, it swells up, how many more times do you bite that same spot on your lip over the next few days? The same thing happens with the IT Band. Repeated run-ins with the femoral epicondyle can cause the IT Band to increased damage beyond friction and inflammation. It will eventually scar over, and that scar tissue is much less malleable and flexible than the band itself. When scar tissue is created over the friction location, it becomes tighter and more susceptible to further complications with friction. This can wreak further havoc on your knee if you let it go far enough. Eventually the IT Band becomes so tight that it pulls the patella (kneecap) laterally and renders it incapable of tracking properly. This can result in improper wear of the articular cartilage on the underside of your patella and predispose you to run-ending pain. Welcome to Painville… Population: YOU!!!
Signs and Symptoms of IT Band Syndrome
Signs and symptoms of ITB can include, but are not limited to:
- Swelling on outside of knee
- Pain on outside of knee
- This pain is usually characterized by “a sharp stabbing pain” I’ve often heard it described, and what I felt when I had it as “someone is sticking a knife in my knee and twisting it”
- This pain usually presents itself during a run. Usually the first few minutes are tolerable, but the pain is usually great enough that it forces you to stop running.
- Upon standing after sitting for prolonged periods of time
- Upon examination, tight hips are discovered.
- A ‘positive’ Trendelenburg gait
- A physical examination finding associated with various hip abnormalities (those associated with abduction muscle weakness or hip pain) in which the pelvis sags on the side opposite of the affected side during single leg stance on the affected side; during gait, compensation occurs by leaning the torso toward the involved side during stance phase on the affected extremity
- A ‘positive’ Noble Compression Test
- The athlete lies on a table with his/her hip and knee flexed. The athlete slowly extends the injured leg while pressure is applied to the IT band just proximal to the lateral epicondyle of the femur. If the test is positive, the athlete would have significant pain while straightening his/her leg.
- A ‘positive’ Ober’s Test
- The athlete lies on his/her uninjured side with the leg in slight flexion to help maintain balance. The injured leg is passively abducted and slightly extended and then slowly brought back down. If the IT band is tight, the leg will remain in an abducted position.
- A ‘positive’ Trendelenburg gait
Prevention of Illiotibial Band Friction Syndrome can be accomplished in a few easy steps:
- Make sure you have adequate footwear. Check out our gait analysis, we can make sure you have the right shoes. If you pronate you could stretch out the IT Band making it more susceptible to further injury
- Strengthen your hips. Because your hips are responsible for literally thousands of steps a day, you want them to be finely-tuned-athletic-machines. The muscles that are associated with ITB are responsible for hip abduction, so abduct your hips. I’ll tell you how:
- Grab a resistance band. Tie the two ends together so you now have a big rubber band. Take a wide stance with your feet and step on one side of the band, with the side that you’re not stepping on, bring it up to your chin. The rubber band should be making a big triangle if you did it correctly. Keeping the wide stance that you have, walk in a big square pattern always facing the same direction. So you will be walking forwards, sideways, and backwards to complete the square. If this is done correctly, you should feel this in the outside of your hips.
- For hip stability the following exercise is my favorite. Standing on one leg, and the other leg out in front of you, trace a circle one direction for a total of 5 circles, then reverse direction. Then cock your leg out to the side and do 5 circles one direction, 5 circles the other direction. Lastly, kick that leg behind you and do 5 circles one way, 5 the other. Then switch legs. Repeat this several times. The beauty of this is that you can feel your hips working in both legs at the same time!
Rehabilitation
Rehabilitation for the friction syndrome is similar to prevention.
- All the strengthening exercises performed in the prevention section can apply to the rehabilitation section. The more productive and aggressive you are in rehabilitating this injury, the stronger and less injury prone it will become.
- Foam rolling/trigger point massage can be painful but very advantageous.
- The goal with foam rolling is to target the IT Band, AND the muscles from which the Band originate. Roll from your hip all the way down to your knee, and back to your hip. This is 1 (one) repetition, complete 3 sets of 10 as many 3-4 times a day. This is an aggressive injury, you must be aggressive in your rehab if you want to get rid of it!
- COMMON MISTAKE IN FOAM ROLLING – making yourself too comfortable. The goal is not to just roll through the motions, but to actually make a difference. Put as much weight on your affected leg as possible. Relax your affected leg as much as possible. If you tighten your quadriceps muscles while rolling, you are guarding your IT Band and cannot penetrate it deeply at all. Suck it up, embrace the pain, don’t be afraid to shed a tear or two, bruise your leg from rolling. That’s the drawback to the foam roller, it is difficult to inflict pain on ourselves. If this is the case, call me, and we’ll sort this whole thing out!! I’ll bring over my ‘sharp-as-nails’ elbows and go to town on those Bands.
- The goal with foam rolling is to target the IT Band, AND the muscles from which the Band originate. Roll from your hip all the way down to your knee, and back to your hip. This is 1 (one) repetition, complete 3 sets of 10 as many 3-4 times a day. This is an aggressive injury, you must be aggressive in your rehab if you want to get rid of it!
Self-diagnosis can be difficult on this one. If you have any questions, comments, or concerns please feel free to contact me at the Salt Lake Running Company in Draper. 801-676-0844. If you are having hip issues and are concerned whether it is ITB or not, some other things can be going on inside your hips, here’s a quick glance at some other injuries that are sometimes confused with and related to ITB:
Snapping Hip Syndrome
If you feel like your hip snaps from time to time while running, walking or other activity it could be caused by an inflamed bursa sac in your hip. A bursa sac is a fluid-filled sac that helps lubricate a particular joint. If your hip muscles become too tight they can rub on this bursa sac causing it to become inflamed. An inflamed bursa sac is known as bursitis. This type of hip bursitis occurs on your trochanter, which is where the leg bone attaches to the hip. Therefore, this injury is known as Trochanteric Bursitis.
Please post any comments if you have had luck with alternate rehabilitation, modalities, or prevention for Illiotibial Band Friction Syndrome.